Increased admissions lead to greater burnout in Emergency Departments
Extensive hours, late nights and disproportionate patient-staff ratios: Issues that were once meant to be tackled on a short-term basis have now become the standard for emergency departments.
Nearly two years following the initial breakout of the COVID-19 pandemic in the United States, emergency departments struggle to treat the fluctuating amount of incoming patients. With many non-COVID patients avoiding hospital visits in the spring of 2020, emergency rooms saw their caseloads cut in half. By fall 2021, however, patient load has not only returned to normal, but now there is often not enough staff to cover the increase.
Higher-Acuity Cases, Less Staff Capacity
The pandemic caused a conundrum for those patients seeking their conventional doctor visits, causing many to put their ailments on hold. As a result, symptoms have worsened for many and patient care has become more involved. EDs are now facing a snowball effect: increased and more complicated cases, with not enough nurses or staff to spare.
As noted in a recent KHN article, staffing challenges have reached serious levels for some emergency departments that are unable to provide rooms, leading to overflow in hallways and waiting areas. With admission rates 20% higher than average, EDs are forced to stack stretchers in the halls as they work to treat patients urgently awaiting care during peak hours.
A September 2021 commentary from the NEJM Catalyst writes that “there is incontrovertible evidence that ED crowding leads to significant patient harm, including morbidity and mortality related to consequential delays of treatment for both high- and low-acuity patients.” Those prolonged stays also result in higher costs of care, creating an additional financial burden for providers.
The Rising Cost of Burnout
No one knows these pressures better than the ED doctors and nurses working on the frontlines. While one-third of nurses had reported burnout before the pandemic, the statistic is now closer to one-half. And many of these staff members are leaving the industry for better-paying jobs, sometimes tripling their pay for half of the stress.
In the 2022 Environmental Scan by the American Hospital Association, turnover in EDs has increased to 30% in 2021, while the usage of agency nurses and temporary labor has increased by 132% for full-time workers. With every sector of the hospital facing labor shortages, including nurses and techs, Emergency Departments have felt the added pressure.
The key culprit of these burnout effects were not only a result of COVID-19. Clerical duties, including charting and paperwork, are identified as the number one reason for burnout, according to 60% of polled physicians in a recent Medscape survey.
The weight of responsibility to cover these tasks without additional personnel takes a toll on doctors, with 33% of doctors stating additional support staff would make a difference in their workload. Documentation challenges, leading to peak levels of burnout, results in a perfect storm that leaves physicians and nurses left to wonder how they can provide the imperative care their patients need.
Taking on the Burden
When ScribeAmerica launched 20 years ago, the sole focus was to relieve emergency departments of burdens like those described above by providing scribe documentation services. As inputting documentation, flow management, coordinating referrals and multitasking remain the most time-consuming tasks, physicians continue to lose out on quality time dedicated to the patient’s bedside. Now, more than ever, scribes play a crucial role in reducing burnout rates and alleviating the stress load for emergency departments.
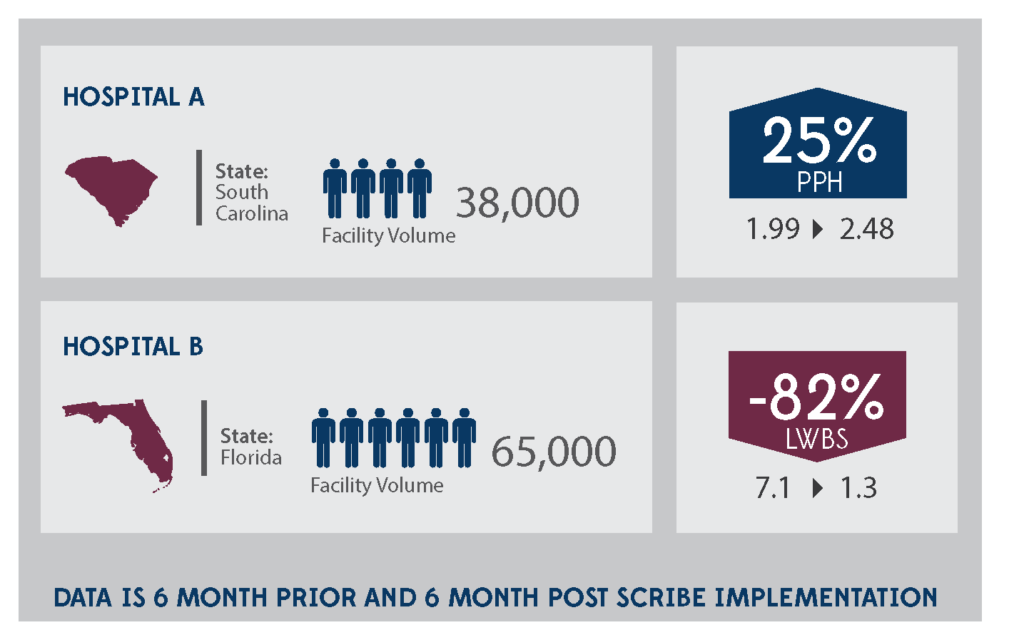
Not only do scribes allow for improved efficiency of provider teams, but they allow physicians to see patients in a more timely manner with reduced clerical burden. In a six-month study run in a South Carolina ED, physicians were able to see 25% more patients per hour as a result of working with scribes. Those patients who had left without being seen (LWBS) had decreased by 82% in one hospital in Florida.
In addition to increased productivity, utilizing an innovative and personalized scribe-enabled model allows cost savings to be passed on to the provider. A 2019 study reports that scribes saved hospitals $31.15 per scribed hour. “Given the strong preference of physicians for working with a scribe, no effect on patient experience, minimal risk, and the productivity and throughput gains outline,” the study states, “Emergency department and hospital administrators should strongly consider the potential utility of scribes in their workforce and financial planning.”
Looking ahead, the AHA expects patient volumes across provider settings to continue to increase. Staffing shortages continue to exacerbate documentation and other administrative challenges, proving the need for services like medical scribes to offer support to providers who need it most, now more than ever.
With continued uncertainty, issues like staffing and provider burnout continue to be top of mind for healthcare leaders. ScribeAmerica continues to provide scribe services needed to reduce those burdens, increase efficiency and get providers back to the bedside instead of behind the computer.
To learn more about customized scribing programs for Emergency Departments, please visit our Emergency Scribes page.



