Value in healthcare ultimately provides the best quality of care for patients, but also allows healthcare providers to reap the rewards of their hard work. The key to accomplishing this is in understanding and mastering the two sometimes-opposing elements of efficiency and time to produce the ideal goal — care that is effective and productive (in the form of cost-effectiveness and revenue) at the same time.
The push for quality via value
The key to finding efficiency lies in value, and that’s exactly the direction that the Centers for Medicare and Medicaid Services (CMS) have been pushing providers, facilities and healthcare systems towards. Recent government initiatives and information technology efforts, such as those surrounding electronic health records (EHRs), are designed to encourage creative thinking around quality innovation. Patients, too must feel valued by the way care is delivered. In an ideal world, everyone — government, providers of healthcare, and patients — would benefit.
Variables in continuous improvement: the quality matrix
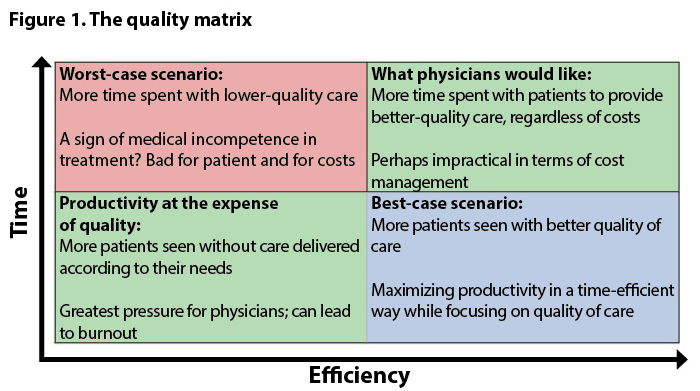
The combination of time and efficiency makes for quality. Physicians tend to focus on time spent as the key to improving patient care. On the other hand, the goal of healthcare management is to optimize productivity and find ways to increase revenue and avoid penalty costs, which is often achieved by reducing the amount of time spent per patient. Both cases have a point, and both are important. It’s therefore important to not look at either one individually as “good” or “bad” but, rather, to find ways they can intersect (Figure 1).
In this view, there are four basic scenarios, plotted into quadrants.
The worst-case scenario – Where physicians spend more time working, they aren’t necessarily able to get more done, particularly if they spending too much of that work time on administrative tasks, or do not have easy access to the right pathways and partnerships to ensure high-quality patient care. Using certified medical scribes is one way to reduce the workload that eventually leads to burnout. In addition, embracing integrated care partnerships and a population health approach can minimize the headaches of logistics for physician and patient alike, helping patients to get the right care at the right time.
The moderate-case scenarios – In one, too much time is spent to achieve productivity; in the other, patients are being seen quickly and often. In the former scenario, support such as scribes and honing of partnerships can help maintain efficiency while decreasing time. In the latter, the fix is the same, only with the goal of giving physicians more one-on-one time with patients. As few providers and practices are operating in “worst-case scenario” territory, these two are where most fall. And, in part, that’s the fault of the traditional payment structures of CMS and private payors: providers and facilities have historically been rewarded for volume of care via fee-for-service payments. At whatever cost to time or efficiency. That’s what CMS is changing with accountable care organizations, bundled payments and the new impending physician fee structure.
The best-case scenario – This is where the patient gets the right treatment, at the right time, for the right amount of time, with as little waste as possible. The CMS hospital readmissions program is a great example. Readmissions are costly, time-consuming and, often, more medically complex. CMS doesn’t want hospitals to simply turn patients away to avoid penalties but, rather, to ensure patients receive the right care during admission, are connected to the appropriate post-acute care after discharge, and are given thorough, empowering education that engages them in decision-making about their health. Although patients might spend a bit longer in the hospital on the front end, the time saved in securing post-acute care and in spending time in the hospital later mean that care is vastly more efficient on the whole — not to mention of higher quality.
Disruption is the key
It’s not perfect yet — there are always going to be rough patches when change occurs. But, overall, CMS’s efforts are working. The key is to gather and analyze strong data to drive decision-making and to think disruptively about healthcare delivery in terms of how it can be structured. Time and productivity are not at odds with one another; they’re forces for driving change by finding ways to both.