Last week’s post dealt with the very complex epidemic of medical errors in the U.S., which causes truly unacceptable morbidity and mortality. One of the factors identified was the lack of adequate training and up-to-date education of physicians in a rapidly changing landscape of healthcare and medical technology. There appears to exist a large gap between “what I have been doing” and “what I should be doing” for optimal patient care. The requirement by state medical and specialty boards for continuing medical education (CME) has long been established as the gold standard in ensuring doctors remain current within their particular specialties. The Accreditation Council for Continuing Medical Education (ACCME) was founded in 1981 with the purpose of setting and maintaining long-term physician-education requirements. Obviously, a doctor has not learned all they will ever need to know upon receipt of his/her MD diploma. John Shaw Billings noted over a century ago that “the education of the doctor which goes on after he has his degree is, after all, the most important part of his education.”
However, are one week getaway cruises to exotic destinations — complete with hours of flashy PowerPoint presentations and didactic teaching — really effective in changing the way physicians care for their patients? Is there any evidence of improved patient outcomes? Traditional CME typically mimics medical school lecture halls, force-feeding facts to passive recipients. In September 1999, about 7 years before sweeping reform of CME took place, JAMA published the results of several carefully designed studies that clearly showed “didactic sessions do not appear to be effective in changing physician performance,” hence no change in patient outcome. In contrast, it was shown that interactive sessions requiring active participation along with the opportunity to actually “practice” in the process of learning, at times did improve physician performance and patient outcomes.
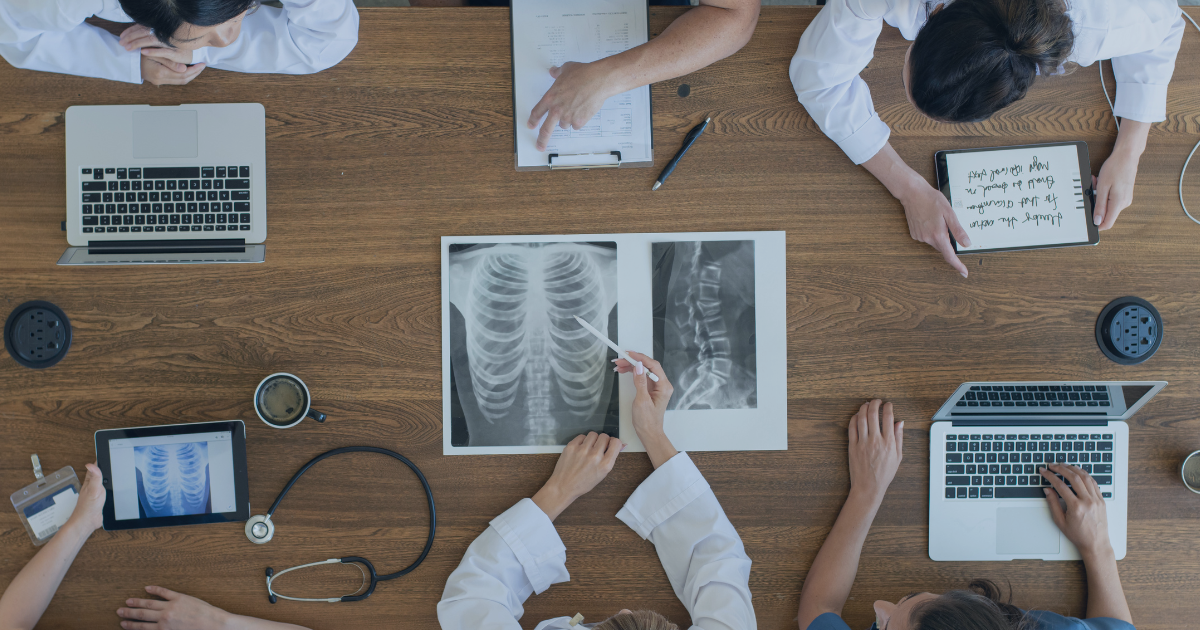
In 2006 the ACCME published new accreditation criteria that did not replace but rather added to previous guidelines for CME, to create a more learner-centered approach. The “new and improved” CME has been designed to not only mix and match various forms of teaching to the different ways physicians learn new information, but to also ensure new knowledge is translated into behavior change. Additionally, any accredited provider must provide mission statements, use a needs assessment in planning CME activities, provide clear objectives, and have a way of evaluating the CME program’s effectiveness in promoting real change. Clearly, CME has become enriched and creative, which can actually lead to real change in physician practice standards. Interactive learning is now becoming the norm within the CME industry. Specific examples might include case discussions, role-play, and hands-on practice sessions.
Effective CME can clearly help physicians improve practice standards and patient care, however “left to their own devices,” most busy doctors would have difficulty organizing and maintaining their ongoing education. Therefore, there exists a strong alignment between CME, Maintenance of Certification, and Maintenance of Licensure. There is a requirement to obtain yearly CME hours in order to be licensed by a medical board or certified within a given specialty. In other words, the privilege of practicing medicine must go hand in hand with the obligation of being a lifelong student. The phrase “continuous professional development” in some cases has replaced the term CME when the emphasis is more on lifelong, continuous, individualized, learner-centered education that covers the full spectrum of a given specialty using various formats and media.
The idea of training physicians over their careers, beyond medical school, is as old as the profession itself. After all, one of the attributes that often drives an individual into medicine is the need, perhaps even compulsion, to know by way of learning. What has changed in the past decade are the ways CME is delivered. Certainly, the rise in medical errors along with the tremendous growth in medical science have served as catalysts in helping us find a better, more practical, more effective way of continuously educating our doctors throughout their professional lives.